Cancer is characterized by uncontrolled cell proliferation, resulting in the loss of regulated division, differentiation, and apoptosis. As a global health burden, cancer remains one of the leading causes of mortality and contributes to decreasing life expectancy worldwide. According to the International Agency for Research on Cancer, nearly 19.3 million new cancer cases and approximately 10 million cancer-related deaths were anticipated by 2020. The five most commonly diagnosed cancers include female breast cancer (11.7%), lung cancer (11.4%), colorectal cancer (10%), prostate cancer (PC; 7.3%), and stomach cancer (5.6%).
Prostate cancer (PC) is a non-cutaneous malignancy predominantly found in males over 50 years of age, impacting approximately 1.6 million individuals and accounting for over 300,000 deaths worldwide. It ranks as the second most frequently diagnosed cancer in men and the fifth leading cause of cancer-related death. In India, PC was reported as one of the most common cancers in 2020, with 41,532 new cases, representing 5.7% of total male cancer diagnoses. The risk of being diagnosed with PC in Indian men stands at approximately one in 125. The increase in PC incidence over recent decades has been largely attributed to the widespread use of prostate-specific antigen (PSA) screening, which has played a significant role in reducing mortality among diagnosed cases. Early diagnosis and advancements in treatment have been pivotal in decreasing PC mortality rates.
The prostate is a walnut-sized gland located in the male pelvis, responsible for secreting seminal fluid that nourishes and transports sperm. This fluid also contains an alkaline solution aiding sperm survival in the acidic environment of the vagina. The most common type of PC is adenocarcinoma, accounting for 90–95% of cases. Other types include squamous cell carcinomas, transitional cell carcinomas, neuroendocrine tumors, and prostate sarcomas. The incidence of PC increases significantly with age, with risk factors including race, ethnicity, diet, obesity, family history, and smoking.
Clinical symptoms of PC vary depending on the stage of the disease. Early-stage PC may present with urinary symptoms such as a painful and poor urinary stream, frequent urination, erectile dysfunction, painful ejaculation, and hematuria. Advanced stages may lead to metastasis, commonly affecting the vertebrae and resulting in chronic back and hip pain, sometimes linked to Pott’s disease. Urinary incontinence is another symptom observed, particularly following radical prostatectomy in early-stage PC.
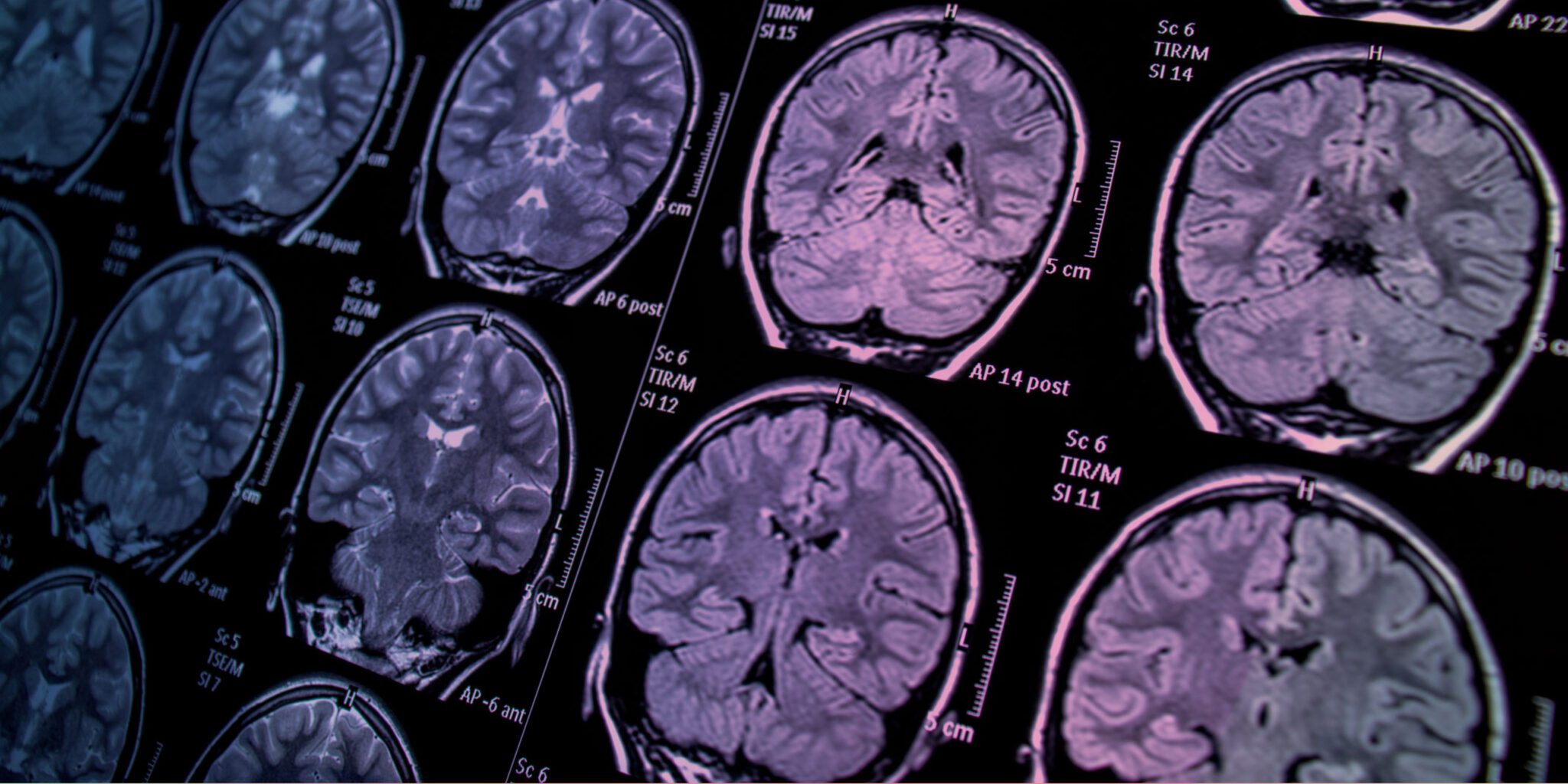
For early detection of PC, PSA screening is recommended for men aged 55–69. In cases where PSA levels are elevated, a digital rectal examination (DRE) is performed. If warranted, a systemic prostate biopsy can be conducted using transrectal ultrasound (TRUS), transperineal biopsy, multiparametric magnetic resonance imaging (mpMRI), or targeted MRI-ultrasound fusion biopsy. The Gleason grading system is employed to grade tumors, aiding patients in selecting appropriate therapeutic options. Recent advancements include the use of mpMRI before biopsy, particularly beneficial for biopsy-naive patients, and non-invasive techniques such as liquid biopsy for tumor detection.
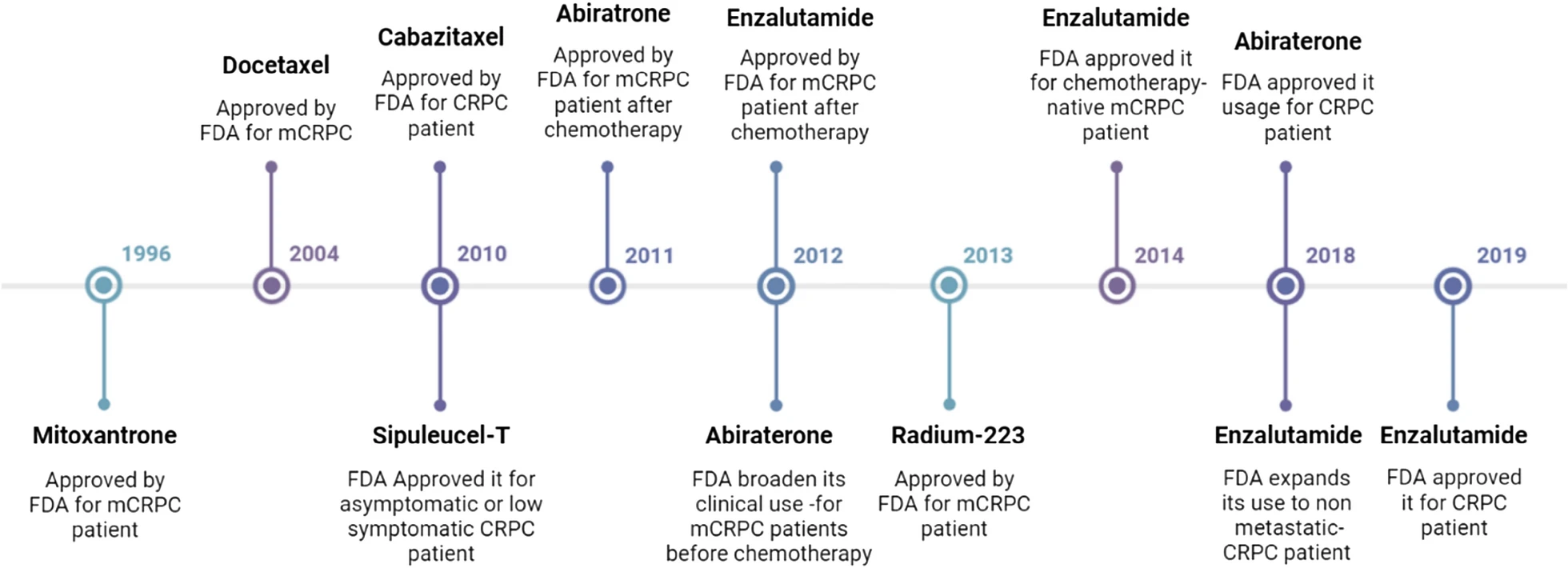
Therapeutic approaches for PC include both pharmaceutical and surgical treatments. One significant advancement in PC treatment is the inhibition of the androgen signaling pathway, which reduces androgen levels through hormone-based treatments known as androgen deprivation therapy (ADT). ADT has proven highly effective for treating metastatic hormone-sensitive PC (mHSPC) and may eventually lead to metastatic castration-resistant PC (mCRPC). Approved drugs for ADT include abiraterone acetate and enzalutamide. Chemotherapeutic options consist of docetaxel, cabazitaxel, and mitoxantrone, while radioisotopes like radium-223 are used in cancer treatment. These drugs have received approval from the United States Food and Drug Administration (US FDA).
Surgical interventions are often effective for localized PC, contributing to long-term survival. However, PC survivors may experience significant impacts on quality of life (QoL). Common issues include depression, as well as physical and sexual dysfunctions. Addressing these challenges is essential for improving the well-being of PC survivors.