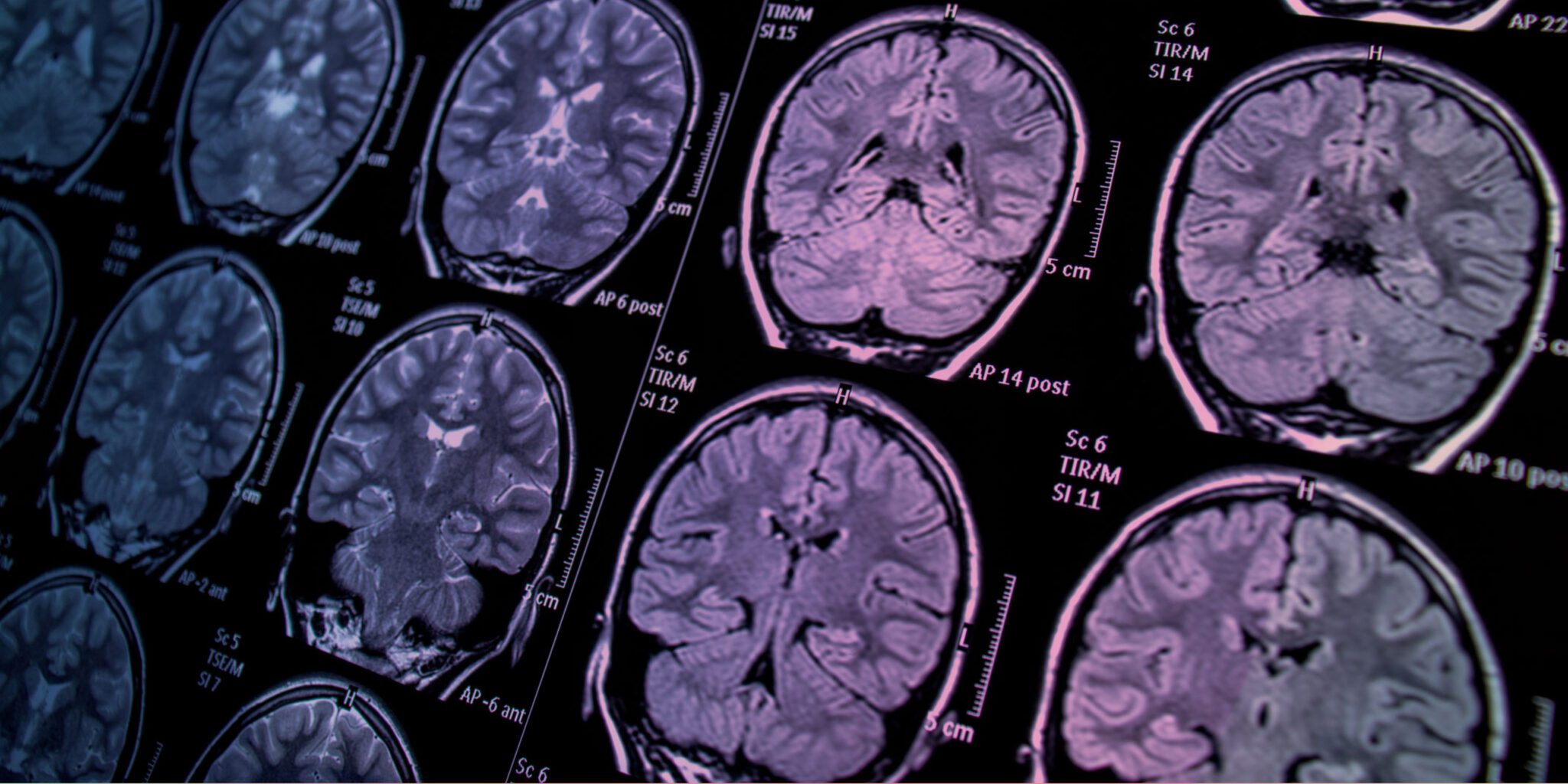
Recent years have brought remarkable progress in oncology, particularly in diagnostic imaging technologies, which have significantly impacted patient care, including advancements in cervical cancer (CCa) management. The curated Research Topic titled “Breakthroughs in Cervical Cancer Imaging” features five pivotal papers that highlight innovations aimed at enhancing prediction and diagnosis in CCa. This blog post encapsulates the key findings and implications of these contributions, providing insights into future research and clinical practice.
Synthetic MRI and Lympho-Vascular Space Invasion Guo et al. investigated the use of synthetic magnetic resonance imaging (MRI) to assess lympho-vascular space invasion (LVSI) in cervical squamous cell carcinoma cases without lymph node metastasis. Their study demonstrated that quantitative parameters derived from synthetic MRI, such as T1, T2, and proton density maps, could effectively differentiate between negative and positive LVSI groups. This non-invasive method holds potential for assessing tumor aggressiveness and improving diagnostic precision.
MRI and Diffusion-Weighted Imaging for Pelvic Lymph Node Metastasis Fan et al. explored the combined use of conventional MRI and diffusion-weighted imaging (DWI), along with the apparent diffusion coefficient (ADC), for predicting pelvic lymph node metastasis in CCa. Their research revealed that lower tumor ADC values are associated with pelvic lymph node metastasis, suggesting that this imaging method can enhance diagnostic accuracy and assist in better patient management.
Superb Microvascular Imaging for Lesion Differentiation Zhu et al. examined the diagnostic value of superb microvascular imaging (SMI) in distinguishing between premalignant and malignant cervical lesions. The study highlighted that the vascular index measured by SMI has high diagnostic performance, offering a promising non-invasive option for early detection and characterization of cervical lesions.
Integrating MRI Features with Clinical Data for Prognosis Lin et al. focused on developing a comprehensive model that integrates clinical characteristics with MRI features to predict survival outcomes in patients with locally advanced CCa. Their findings indicated that this combined approach significantly enhances the accuracy of prognostic models, facilitating more tailored patient care and personalized treatment strategies.
Contrast-Enhanced Ultrasound and Elastography for Therapy Response Ma et al. assessed the use of contrast-enhanced ultrasound combined with elastography to predict the efficacy of concurrent chemoradiotherapy in CCa. Their study suggested that this imaging combination, alongside tumor marker squamous cell carcinoma antigen levels, could improve predictions of disease progression, supporting advanced imaging’s role in treatment planning.
Implications for Future Research and Clinical Practice The collective findings from these studies mark a significant step forward in imaging applications for CCa. The integration of modern imaging techniques not only enhances diagnostic and staging capabilities but also opens new possibilities for predicting pathological stages, malignancy, treatment response, and overall clinical outcomes. Such predictive capabilities are vital for developing personalized treatment plans, which can improve patient prognosis and quality of life.
The advent of artificial intelligence (AI) in imaging promises further transformation, with AI-driven models enabling more precise and efficient diagnostics in CCa. Emerging fields like radiomics, which involves extracting large sets of features from radiographic images through data-characterization algorithms, offer deeper insights into tumor heterogeneity and could greatly influence treatment decisions and prognostic assessments. Additionally, imaging-based analysis of body composition, focusing on conditions like sarcopenia (muscle mass loss) and sarcopenic obesity (combined muscle loss and obesity), can provide critical information about treatment tolerability and patient outcomes.
Conclusion The research highlighted in this series underscores the pivotal role of comprehensive imaging assessments in CCa care. These advancements reflect not only improved diagnostic and predictive capabilities but also a shift toward personalized, physiologically nuanced approaches to cancer treatment. As we continue to explore these technologies, their integration into clinical practice holds promise for significantly enhancing the management of cervical cancer, paving the way for better outcomes and ushering in a new era of gynecological oncology care.
Reference : Imaging of cervical cancer