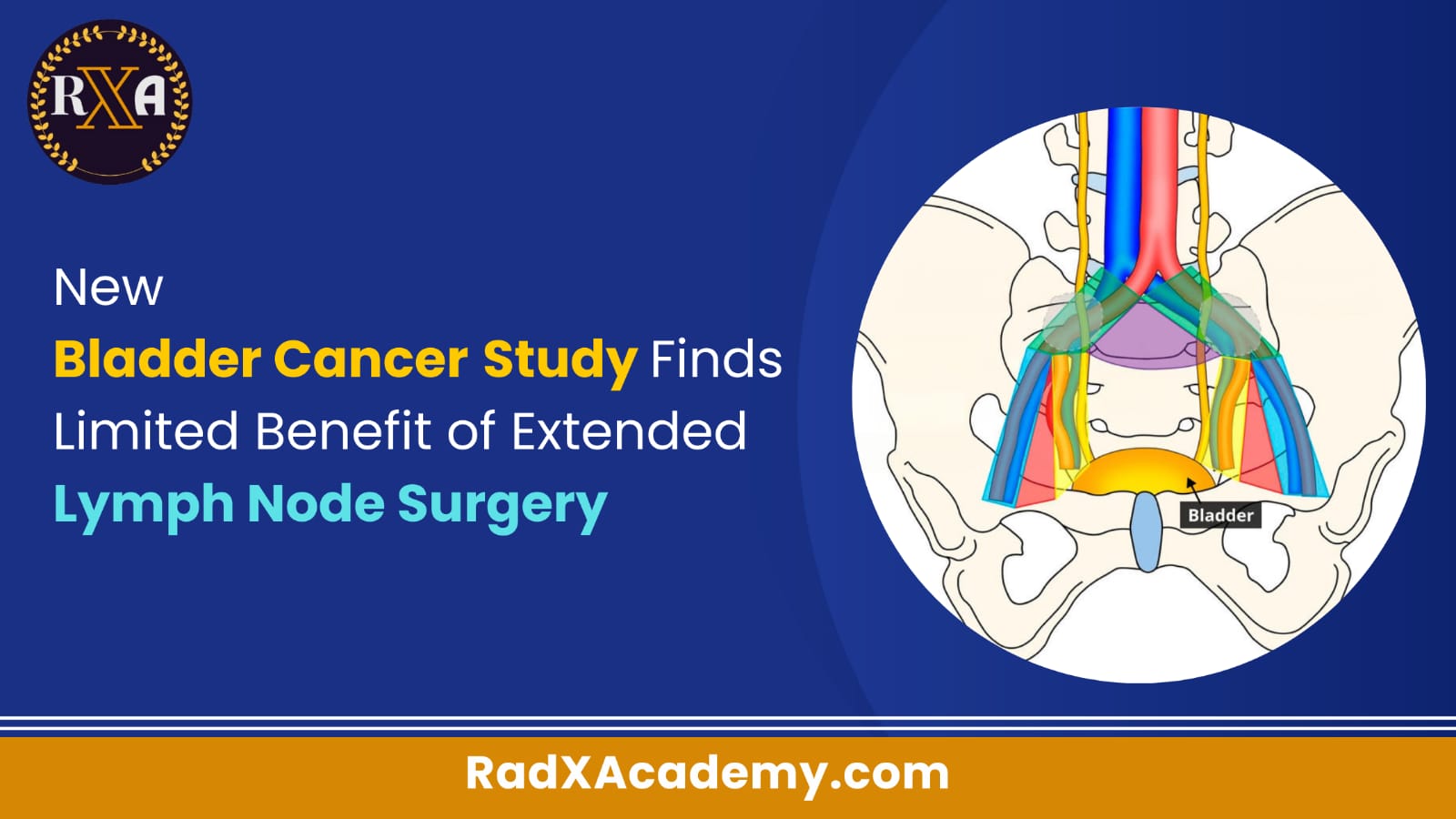
Surgeons often treat certain types of bladder cancer by removing the bladder and nearby lymph nodes, a procedure that helps reduce the risk of cancer returning in the pelvis. For patients with localized muscle-invasive bladder cancer, two main approaches are used to remove lymph nodes during bladder removal surgery: standard lymph node dissection and extended lymph node dissection.
While both types of lymph node surgery are common, few studies have directly compared their outcomes. A notable 2019 clinical trial conducted in Germany found that extended lymph node surgery did not improve survival rates for patients. Now, new research funded by the National Cancer Institute (NCI) has supported these findings, showing no added benefit from more extensive lymph node removal.
This recent trial, led by the SWOG Cancer Research Network, included approximately 600 patients with localized muscle-invasive bladder cancer. Participants were randomly assigned to undergo either standard or extended lymph node dissection during surgery to remove the bladder. After a median follow-up period of 6.1 years, the study revealed no significant difference in overall survival or disease-free survival between the two groups. These results were published in the New England Journal of Medicine on October 2.
Specifically, the trial found that the 5-year disease-free survival rate was 60% in the standard surgery group and 56% in the extended group, while the 5-year overall survival rate was 63% for the standard group compared to 59% for the extended group. However, extended lymph node surgery was associated with a higher risk of serious side effects, including anemia requiring transfusions and wound complications (54% in the extended group versus 44% in the standard group).
The study’s lead investigator, Dr. Seth P. Lerner of Baylor College of Medicine, noted that these findings reinforce the evidence from the German trial, confirming that extended pelvic lymph node dissection does not improve survival outcomes. Dr. Ashish Kamat, director of bladder cancer research at the University of Texas MD Anderson Cancer Center, highlighted that the study could lead to a more selective approach to extended lymph node dissection.
“Less is often more,” Dr. Kamat emphasized. “This study clearly demonstrates that extended lymph node dissection does not enhance survival for most patients but does increase the risk of complications.”
For years, many medical centers have adopted the more extensive procedure despite limited comparative research. These new results underscore the importance of rigorous clinical trials to evaluate surgical practices before they become standard. Dr. Lerner stressed that “when high-level scientific evidence is lacking, we should challenge the conventional wisdom.” Randomized clinical trials like this one are crucial for filling knowledge gaps and guiding medical practice.
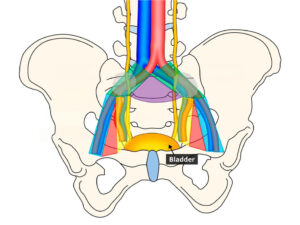
The SWOG trial included experienced urologic cancer surgeons from 27 sites across the United States and Canada. Each participating surgeon had performed at least 50 radical cystectomies over the preceding three years, ensuring a high level of surgical expertise.
Moving forward, Dr. Lerner and his team are analyzing tumor tissue samples from trial participants to identify molecular profiles that could be linked to survival outcomes. Feedback from the medical community since the presentation of these results at conferences in 2023 has been generally positive, with many surgeons expressing relief at not having to perform extended lymph node dissections in suitable cases.
Dr. Kamat believes that the findings will “empower surgeons to avoid unnecessary harm, potentially leading to faster recovery and better quality of life for patients.” This shift towards standard lymph node surgery could mark a significant improvement in patient care, balancing efficacy with safety.
Reference : Extended Lymph Node Surgery Doesn’t Improve Survival