New Research Could Make Radiation Treatment for Lung Cancer More Effective and Less Toxic
In exciting new research, a team from the University of Cincinnati has discovered a potential breakthrough in treating lung cancer that has spread to the brain. Led by Dr. Debanjan Bhattacharya, this study could make radiation therapy more effective, while reducing side effects for patients with lung cancer brain metastases. Their findings, recently published in the journal Cancers, offer hope for improving both the quality of life and survival outcomes for those facing this tough diagnosis.
Understanding Lung Cancer and Brain Metastases
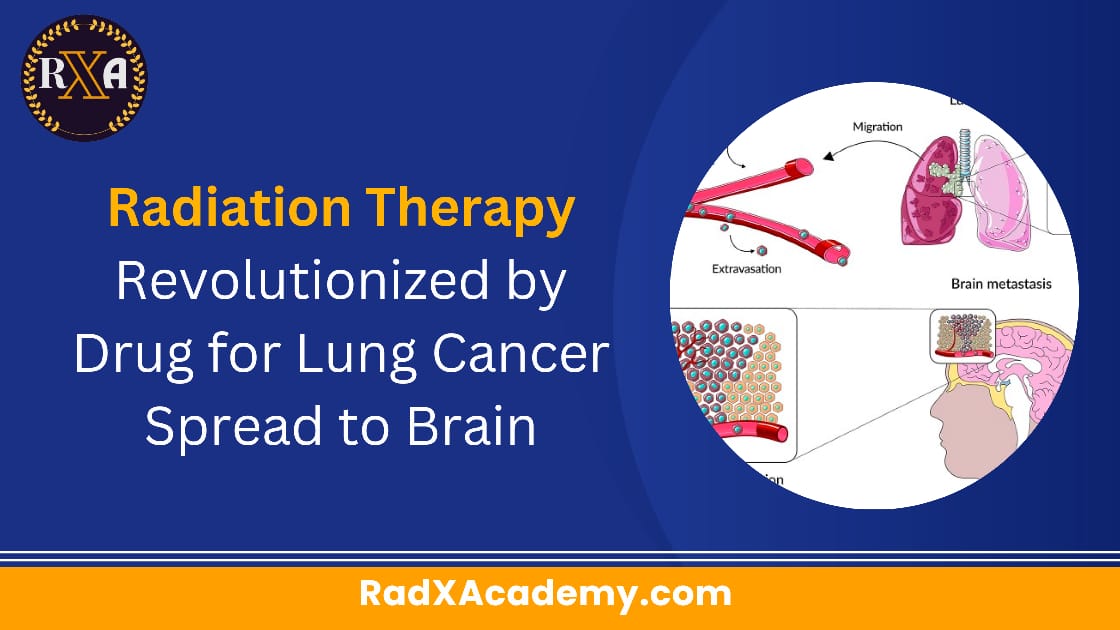
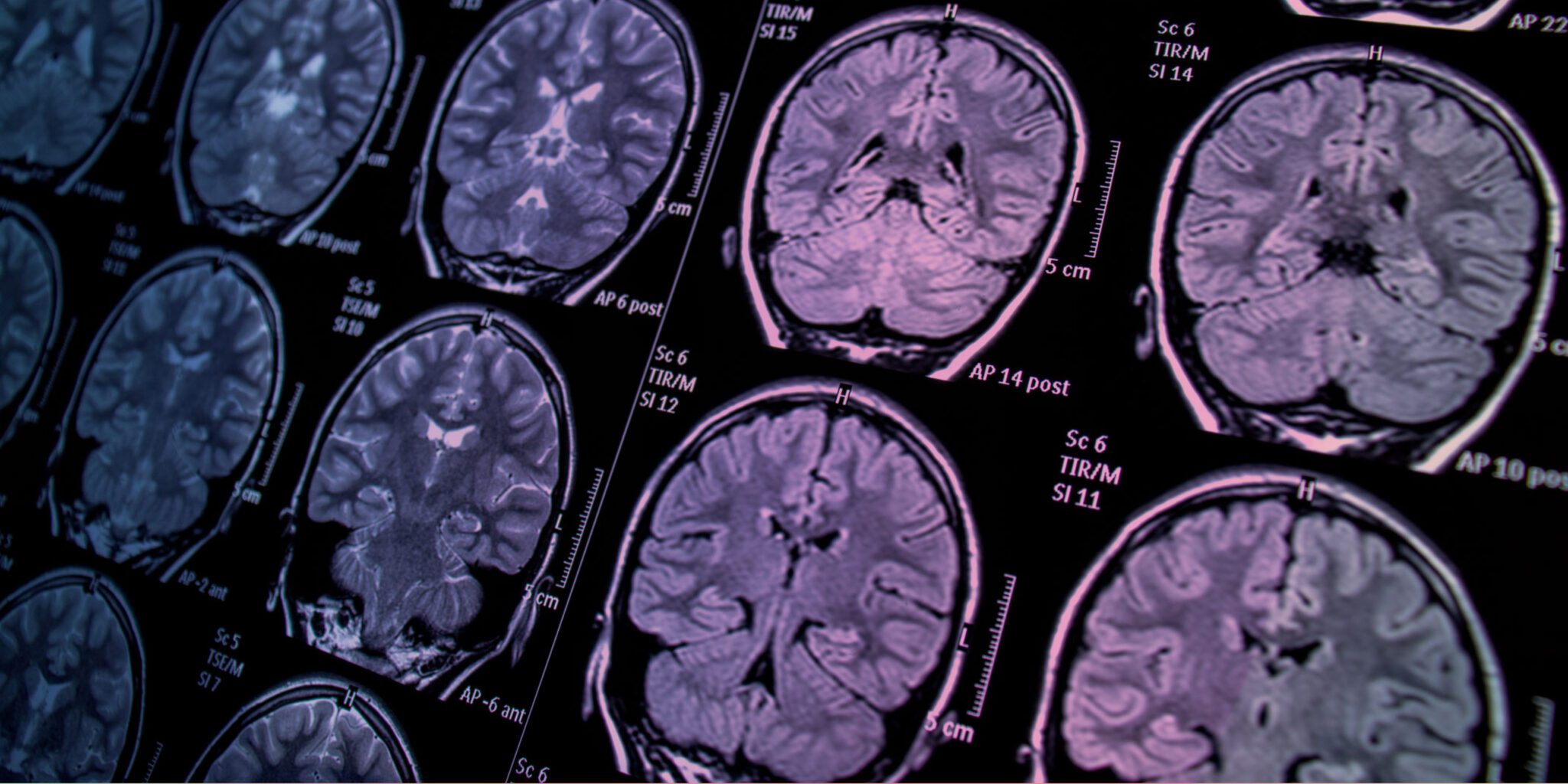
Lung cancer remains the leading cause of cancer-related deaths in the United States, responsible for about 20% of all cancer deaths. Non-small cell lung cancer (NSCLC) makes up the majority of lung cancer cases, accounting for 80% to 85% of diagnoses. Tragically, up to 40% of lung cancer patients will develop brain metastases—secondary tumors that have spread from the lungs to the brain.
Current treatments for brain metastases often include surgical removal of tumors, stereotactic radiosurgery (a focused form of radiation), or whole brain radiation for patients with numerous brain metastases. While these therapies can extend life, they are not a cure, and the survival rate for patients with lung cancer brain metastasis is typically only 8 to 10 months. Additionally, these treatments can cause serious side effects due to the toxicity of the radiation.
A New Approach: AM-101
The research team, led by Dr. Bhattacharya, focused on a drug called AM-101, a synthetic benzodiazepine that has shown promise in previous studies. Benzodiazepines are a class of drugs known for their ability to cross the blood-brain barrier, a protective shield that prevents harmful substances from entering the brain. This is crucial when treating brain metastases, as many drugs fail to reach their target in the brain.
AM-101 had never been tested in the context of lung cancer, but early studies suggested it might help improve radiation treatment for lung cancer patients. The team’s research found that AM-101 works by activating GABA(A) receptors on lung cancer cells and brain metastatic cells. This activation triggers a process called autophagy, where cells recycle and break down damaged or unnecessary components.
By enhancing autophagy, AM-101 made lung cancer cells more vulnerable to radiation. In animal models, the drug improved the effectiveness of radiation therapy, significantly increasing survival rates. It also slowed the growth of both primary lung cancer cells and brain metastases.
Potential Benefits for Patients
What’s especially promising about these findings is that combining AM-101 with radiation could potentially reduce the amount of radiation required, meaning fewer side effects and less toxicity for patients. Since radiation treatment can be harsh on the body, this lower-dose option could lead to better quality of life for patients undergoing treatment.
Dr. Bhattacharya and his team are now preparing to begin Phase 1 clinical trials to test the combination of AM-101 and radiation therapy in humans. These trials will explore the drug’s potential for both treating primary lung cancer and brain metastases.
A Collaborative Effort
Dr. Bhattacharya credits his mentors, Drs. Soma Sengupta and Daniel Pomeranz Krummel, and the collaborative efforts of researchers at the University of Cincinnati and other institutions, for helping make this breakthrough possible. He also emphasizes the role of university research resources that enabled the team to conduct this work.
This research is especially meaningful to Dr. Bhattacharya, as he dedicated the study to his father, who passed away in 2021 during the early phases of the project. His father had been deeply supportive of his research, and his passing motivated Dr. Bhattacharya to work even harder to bring the study to completion.
Looking Ahead
While there is still much work to be done, this study represents a promising step toward improving radiation therapy for patients with lung cancer that has spread to the brain. By combining AM-101 with radiation, there is hope that patients will experience better outcomes with fewer side effects, offering a new ray of hope in the fight against this challenging form of cancer.
As the research moves forward, the hope is that AM-101, combined with radiation therapy, will become a valuable treatment option for patients with lung cancer brain metastases—offering not just increased survival, but a better quality of life.
Reference : Drug Improves Lung cancer that has spread to the brain