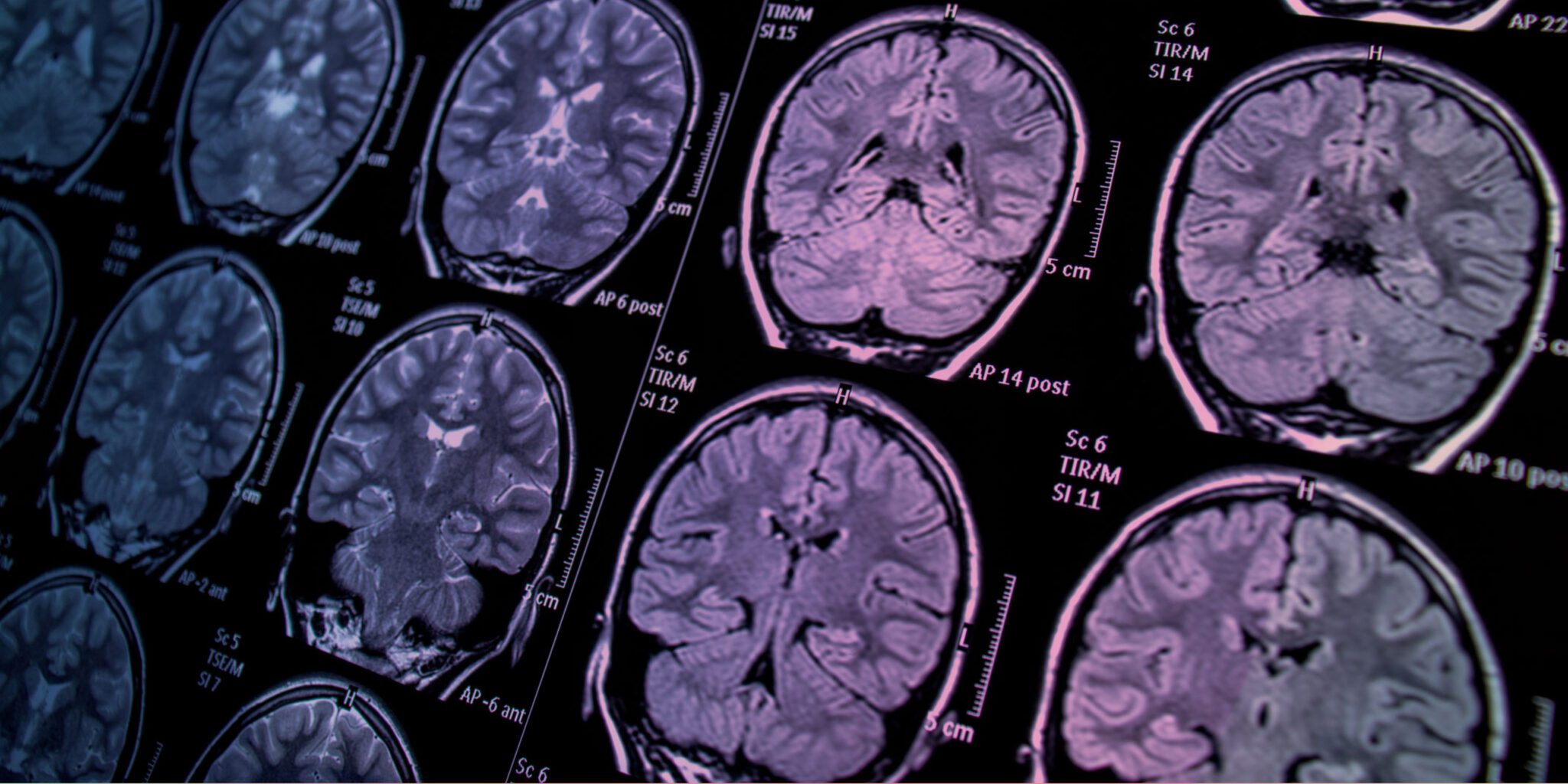
Groundbreaking Immune Therapy Shows Promise for Glioblastoma Treatment
A research team led by Dr. David B. Weiner, Executive Vice President of The Wistar Institute and director of its Vaccine & Immunotherapy Center, has achieved a major milestone in glioblastoma research. Known as the deadliest form of brain cancer, glioblastoma has a grim survival rate of less than 5% over five years. In a study recently published in the Journal for ImmunoTherapy of Cancer, Dr. Weiner and his team revealed the success of a novel immune therapy in preclinical testing. The therapy improved survival rates and reduced tumor burden, offering fresh hope for one of cancer’s most daunting challenges.
Tackling Glioblastoma’s Deadly Complexity
Glioblastoma is notoriously difficult to treat due to its ability to suppress the immune system and its intrinsic diversity, which enables tumors to escape conventional treatments. These challenges highlight the need for innovative approaches to help the immune system recognize and fight glioblastoma tumors effectively.
“All cancers, especially fast-growing and immune-silent cancers like glioblastoma, rely on antigens to remain hidden from the immune system,” explained Dr. Weiner. “In glioblastoma, the diversity of these antigens requires a therapy capable of delivering a vast array of information to the immune system.”
The Power of Trispecific Antibodies
Dr. Weiner’s team designed a revolutionary approach using trispecific antibodies encoded through a DNA-based delivery mechanism called DTriTEs (DNA-encoded Trispecific T-cell Engagers). These DTriTEs are engineered to bind cancer-fighting T-cells through the CD3 protein and target two glioblastoma-specific antigens: IL-13Rα2 and EGFRvIII. This unique mechanism enables the immune system to recognize and combat glioblastoma cells expressing either or both antigens.
In preclinical models, DTriTEs showed exceptional promise:
- Activated both T-cells and Natural Killer (NK) cells, critical for a strong antitumor response.
- Achieved 100% survival and tumor control across multiple short-term testing models.
- In long-term studies, 66% of treated models demonstrated sustained tumor suppression and survival—significantly outperforming comparison treatments.
A Glimpse into the Future
“This study demonstrates the potential for a trispecific antibody to overcome glioblastoma’s resistance mechanisms and trigger a lasting immune response,” said Daniel H. Park, lead author and Ph.D. student in Dr. Weiner’s lab. “Our work is just beginning, and we aim to refine these designs to treat not only glioblastoma but other cancers that evade immunotherapy.”
Dr. Weiner added, “What excites us most is the possibility of deploying this technology directly in patients as a scalable, in vivo therapy. If successful, it could prevent tumor escape mechanisms in glioblastoma and even other cancers in the future.”
Hope on the Horizon
As researchers look toward human trials, this discovery has sparked new optimism for glioblastoma patients and their families. The potential to harness DNA-encoded trispecific antibodies could revolutionize the treatment landscape, paving the way for therapies that transform grim outcomes into stories of survival and recovery.
Stay tuned for more updates as this groundbreaking research progresses. With every step forward, hope grows stronger in the fight against glioblastoma and other resistant cancers.
Reference : Immunotherapy for brain cancer